Persistent pain and physiotherapy

Persistent pain in numbers
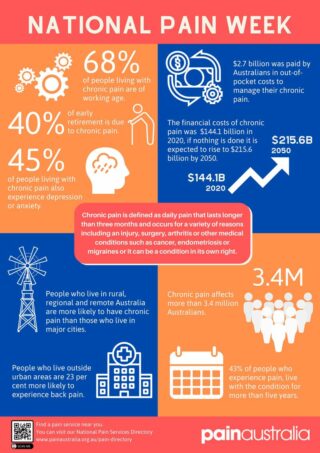
Statistics can be boring, but they paint a picture, so here is one paragraph that sets the backdrop. In Australia, if you stood in a room with 10 randomly-selected people, one of those people is likely to have persistent pain. If these people were all over the age of 45 years, 2 of them would be suffering from persistent pain. In 2020, we know that 3.4 million people lived with persistent pain in Australia, with 53.8% of them being women. 68.23% of them are still working age (that’s 2.3 million people). The financial costs to the person and the healthcare system are well documented, totaling $144 billion (projected to be $215 billion in 2050). Those who live in rural, remote or regional cities are more likely to experience persistent pain. Part of the criteria for having persistent pain is having it for more than 3 months, but we know that 43% of those with persistent pain actually have it for more than 5 years. Work productivity decreases, quality of life decreases and 40% of early retirement is due to persistent pain.
So, is it a real thing?
Sure, numbers are facts. But is persistent pain a real thing given that we can’t see it? Aren’t we just talking about people who can’t cope with their pain? Ok good, so you recognise the loaded nature of these questions. However, they do bring up some important discussion points.
Firstly, persistent pain can be from actual musculoskeletal conditions such as arthritis or nerve compression in the spine. It can also be from medical conditions like migraines, endometriosis or cancer. It is clear that the underlying condition whether it be arthritis, cancer or endometriosis needs to be primarily targeted and managed in order to gain control over the pain experience. Sometimes this involves doctors doing investigations to find the pathology, medications, surgery and physiotherapy. Pretty real stuff so far.
Secondly, we also know that pain can be a primary condition in its own right, such as in fibromyalgia or complex regional pain syndrome. This is recognised in official definitions of pain conditions – https://www.iasp-pain.org
Thirdly, even after the underlying physical, musculoskeletal or medical issue is no longer relevant because you are managing it really well or because you had a treatment such as surgery, we know it is still possible to have a pain issue.
Why does this happen?
There are so many amazing metaphors and stories to illustrate how pain works. As simply as I can put it, the nervous system senses a threat, and sometimes decides to sound the alarm bells, bringing our attention to the threat and motivating us to address it. We also know that there are some factors which amplify the alarm bell response or lower the threshold for the alarm bells to be turned on in the first place. When we understand the whole person (see our previous blog post on the biopsychosocial approach), we can become aware of some of these factors, then come up with a plan that respects or addresses these factors. Ignoring or pushing through these factors can be helpful in the short-term so that we can either avoid pain or achieve a task that may be important to us today. What we see long-term is that either fear-avoiding or doing too much which causes a boom-and-bust pattern of flare-ups both increases the alarm bell response and lowers the threshold for it to be turned on. This makes sense – our body is trying to protect us and senses that we haven’t done enough yet to address the threat. Unfortunately, our alarm bell system can become over sensitive and turn on at inappropriate times, becoming harder to control and turn off.
Can a physiotherapist help?
We may prescribe an exercise to improve your strength, so you stop overloading a part of the body. We may ask you to do relaxation or breathing exercises which allow the nervous system to relax and learn to turn off the alarm bells at the appropriate times. We may help you understand that your current or previous stress, trauma, anxiety or depression is a factor that needs to be managed more optimally. We may educate you about understanding how being neurodivergent or having a hypermobility syndrome influences how your alarm bell system responds.
So, if you feel like any of this applies to you, sometimes you may just need a pain-informed and psychologically-informed physiotherapist to be part of your team and listen to you as an individual, help make sense of your persistent pain experience and collaboratively set up a plan for managing it optimally.
Jamie Chan l Physiotherapist
Lake Health Group
